 Home
Home
 Back
Back
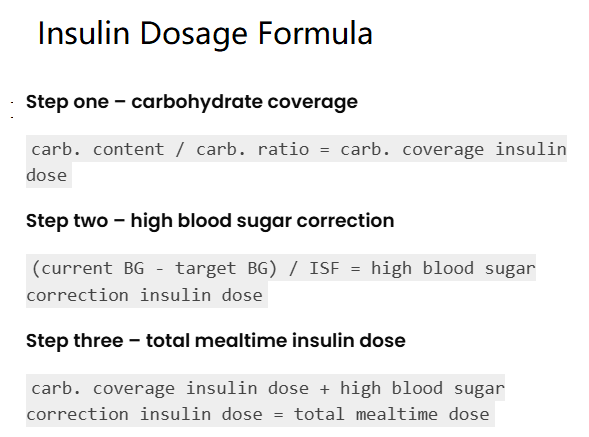
This calculator determines a mealtime insulin dose for patients with diabetes undergoing intensive insulin therapy, based on carbohydrate intake and blood sugar levels, using these formulas:
Step 1 - Carbohydrate Coverage (units):
Insulin Dose to Cover Carbohydrates (units) = Carbohydrate Content (g) / Carbohydrate Ratio (g/unit)
Step 2 - High Blood Sugar Correction (units):
Insulin Dose to Correct Blood Glucose (units) = (Current Blood Glucose (converted to mg/dL) - Target Blood Glucose (converted to mg/dL)) / Insulin Sensitivity Factor (converted to mg/dL/unit)
Step 3 - Total Mealtime Insulin Dose (units):
Total Insulin Dose (units) = Insulin Dose to Cover Carbohydrates + Insulin Dose to Correct Blood Glucose
Where:
This tool estimates a mealtime insulin dose for patients with diabetes undergoing intensive insulin therapy. Input the carbohydrate content of the meal and carbohydrate ratio for Step 1, then current and target blood glucose levels (in mg/dL or mmol/L) and insulin sensitivity factor (in mg/dL/unit or mmol/L/unit) for Step 2. Results show step-by-step insulin doses to cover carbohydrates, correct blood sugar, and the total mealtime dose in units, tailored for individuals on intensive insulin regimens.
Example: Carbohydrate Content 12.36 g, Carbohydrate Ratio 15 g/unit, Current Blood Glucose 150 mg/dL, Target Blood Glucose 100 mg/dL, Insulin Sensitivity Factor 50 mg/dL/unit:
Total mealtime insulin dose:
Step 1 - Carbohydrate coverage:
Carbohydrate content: 12.36 g
Carbohydrate ratio: 15 g/unit
Insulin dose to cover carbohydrates: 0.82 units
Step 2 - High blood sugar correction:
Current blood glucose: 150 mg/dL
Target blood glucose: 100 mg/dL
Insulin sensitivity factor: 50 mg/dL/unit
Insulin dose to correct blood glucose: 1.00 units
Step 3 - Total mealtime insulin dose:
Total insulin dose: 1.82 units
Dosing rules: 0.82 units + 1.00 units
Consult a healthcare provider before administering insulin to ensure it’s safe and appropriate for your diabetes management plan.
Insulin is used to manage type 1 and some type 2 diabetes, replacing or supplementing the body’s insulin to control blood glucose levels, preventing hyperglycemia and related complications.
Mealtime (bolus) insulin is typically taken before meals (2–3 times daily) for patients on intensive insulin therapy, but your doctor will adjust frequency based on your regimen and glucose control.
Rapid-acting insulins like Humalog (insulin lispro), Novolog (insulin aspart), or Apidra (insulin glulisine) are commonly used for mealtime doses, prescribed by your healthcare provider for quick glucose control.
Your doctor or diabetes educator calculates these based on your total daily insulin dose, blood glucose patterns, and response to insulin, often requiring regular monitoring and adjustment.
Track your blood glucose, meals, and insulin doses, then consult your healthcare provider for adjustments to your carb ratio, sensitivity factor, or overall insulin regimen.
Rapid-acting insulin typically starts working in 10–20 minutes, peaks in 1–2 hours, and lasts 3–5 hours, so it’s best taken 10–15 minutes before eating for optimal glucose control.